
Are you taking Spironolactone for your condition but concerned about the risk of pancreatitis? Here’s what you need to know about the potential connection between Spironolactone and pancreatitis.
Understanding Pancreatitis
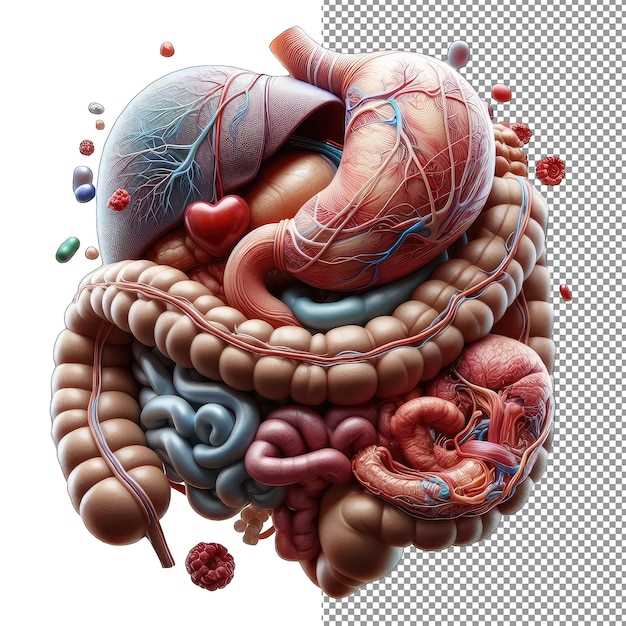
Pancreatitis is a condition characterized by inflammation of the pancreas, a gland located behind the stomach. The pancreas plays a crucial role in digestion and hormone regulation. Pancreatitis can be acute or chronic and can range in severity from mild discomfort to life-threatening complications.
Acute pancreatitis typically occurs suddenly and is often caused by gallstones or excessive alcohol consumption. Chronic pancreatitis, on the other hand, develops over time and is usually linked to long-term alcohol abuse or certain medical conditions.
Common symptoms of pancreatitis include severe abdominal pain, nausea, vomiting, fever, and rapid pulse. Diagnosis is typically made through a combination of physical exams, blood tests, imaging studies, and sometimes pancreatic function tests.
Treatment for pancreatitis may involve hospitalization, pain management, intravenous fluids, and dietary changes. In severe cases, surgery may be necessary to remove blockages or damaged tissue. Managing underlying conditions, such as gallstones or alcohol abuse, is crucial for preventing future episodes of pancreatitis.
Relationship between Spironolactone and Pancreatitis
Pancreatitis is the inflammation of the pancreas, which can be acute or chronic. Spironolactone, a medication commonly used to treat conditions like high blood pressure and heart failure, has been associated with cases of pancreatitis in some patients. While the exact mechanism by which Spironolactone can cause pancreatitis is not fully understood, it is believed that the drug may lead to changes in pancreatic enzymes or bile flow, contributing to the development of pancreatitis.
| Symptoms: | Common symptoms of pancreatitis include severe abdominal pain, nausea, vomiting, and fever. |
| Diagnosis: | Diagnosis of pancreatitis is usually based on clinical symptoms, blood tests showing elevated levels of pancreatic enzymes, and imaging studies like CT scans. |
| Treatment: | Treatment of pancreatitis often involves hospitalization, fasting to rest the pancreas, intravenous fluids, pain management, and addressing the underlying cause, which may include discontinuing medications like Spironolactone if suspected to be the trigger. |
Relationship between Spironolactone and Pancreatitis
Spironolactone, a medication commonly used to treat conditions such as high blood pressure, heart failure, and edema, has been associated with rare cases of pancreatitis. Pancreatitis is a condition characterized by inflammation of the pancreas, which can cause severe abdominal pain, nausea, vomiting, and other digestive issues.
Studies have suggested that there may be a potential link between the use of spironolactone and the development of pancreatitis in some patients. While the exact mechanism is not fully understood, it is believed that spironolactone may trigger an inflammatory response in the pancreas, leading to the development of pancreatitis.
Symptoms of Pancreatitis

The symptoms of pancreatitis can vary from mild to severe and may include abdominal pain that radiates to the back, nausea, vomiting, fever, and rapid pulse. It is important to seek medical attention if you experience any of these symptoms while taking spironolactone.
Diagnosis and Treatment
| Diagnosis | Diagnosis of pancreatitis usually involves blood tests, imaging tests such as ultrasound or CT scan, and sometimes a pancreatic biopsy to confirm the diagnosis. |
| Treatment | Treatment for pancreatitis may involve hospitalization, intravenous fluids, pain management, and addressing the underlying cause, such as discontinuing spironolactone if it is believed to be the trigger. |
Symptoms and Diagnosis
When it comes to pancreatitis, early detection is crucial for successful treatment. Some common symptoms of pancreatitis include severe abdominal pain, nausea, vomiting, fever, and a rapid heartbeat. If you experience any of these symptoms, it’s important to seek medical attention immediately.
Diagnosis
Diagnosing pancreatitis involves a combination of physical exams, blood tests, and imaging tests like ultrasound, CT scans, or MRIs. Your healthcare provider may also perform an endoscopic ultrasound to get a closer look at your pancreas and surrounding organs. It’s important to work closely with your healthcare team to determine the best course of action for treatment and management.
Treatment and Management
Once pancreatitis has been diagnosed, treatment and management focus on addressing the underlying cause and providing supportive care to alleviate symptoms and prevent complications. This may include:
1. Hospitalization: Severe cases of pancreatitis often require hospitalization for close monitoring, intravenous fluids, and pain management.
2. NPO status: Patients may be placed on a “nothing by mouth” (NPO) status to allow the pancreas to rest and recover.
3. Pain management: Pain medications may be prescribed to help alleviate abdominal pain and discomfort.
4. Addressing the underlying cause: If pancreatitis is caused by medications like Spironolactone, the medication may be discontinueied or adjusted under medical supervision.
5. Nutritional support: In severe cases, patients may require intravenous nutrition to ensure they receive adequate nutrients while the pancreas heals.
6. Follow-up care: Regular follow-up appointments with healthcare providers are important to monitor recovery, manage symptoms, and address any complications that may arise.
